“It’s estimated that between 15-30% of hospitalized COVID-19 patients will have detectable new-onset thyroid dysfunction.”
It’s a good time to review the data on how COVID-19 infection impacts the thyroid, and conversely on how existing thyroid disease may impact the risks associated with COVID-19 infection. This is not as easy a task as one might think. An unprecedented number of medical journal articles have been published related to COVID-19 with more than 86,883 publications.
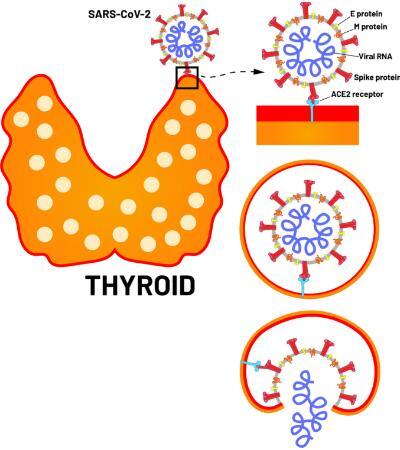
Fig.1 ACE-2 receptors in thyroid follicular cells and SARS-CoV-2 entry
In reviewing this database, there have been approximately 114 publications that are in some way related to the thyroid and COVID-19. Some themes have emerged. I am going to share with you my interpretation of these data. This is not a formal meta-analysis or even a formal literature review. This is an attempt to make some clinically relevant observations from this information.
Do pre-existing thyroid conditions (i.e. hypothyroidism, Hashimoto’s thyroiditis, Graves’ Disease) predispose a person to COVID-19 infection or worse outcomes if infected? This is one of the more commonly asked questions from patients. Because many thyroid conditions are autoimmune disorders, patients wonder if that puts them in the “immunocompromised” category when it comes to COVID-19.
Autoimmune thyroid disease is not an immunocompromised state, so having Hashimoto’s or Graves’ does not put a person in the CDC high-risk category. If a person with a thyroid condition contracts COVID-19, do they have worse outcomes? One of the largest studies addressing this question is a retrospective study of over 3,700 COVID-19 patients in New York City. The study specifically looked at all patients who had pre-existing hypothyroidism and were taking thyroid hormone medication before their COVID-19 infection.
The study found that having hypothyroidism and being on thyroid hormone replacement did not change rates of hospitalization, mechanical ventilation, or mortality relative to those who did not have hypothyroidism. Given this, it seems that a history of hypothyroidism does not change the risk of infection nor the severity of infection with COVID-19. Other smaller studies on this topic seem to corroborate these findings.
The next relevant question is whether COVID-19 infection has any effect on the thyroid gland. With the exception of case reports of subacute thyroiditis, most of these studies are almost exclusively case series of hospitalized COVID-19 patients, so the conclusions are mostly relevant to those patients who were sick enough to be hospitalized. COVID-19 infection does cause thyroid dysfunction, but only in a minority of those infected.
There are two types of thyroid dysfunction that seem to be clearly related to COVID-19 infection: hypothyroidism due to non-thyroidal illness syndrome and thyrotoxicosis (hyperthyroidism) due to subacute (viral) thyroiditis. Neither of these entities are novel to COVID-19, and reasonable explanations for why they occur during COVID-19 infections exist. Non-thyroidal illness syndrome presents as an acute hypothyroid state and subacute thyroiditis presents as an acute subclinical hyperthyroid state. However, in up to 50% of subacute thyroiditis cases, patients can show signs of overt thyrotoxicosis.
Several case series have shown that non-thyroidal illness syndrome can occur in acute COVID-19 infection. The syndrome, also known as euthyroid sick syndrome or low T3 syndrome, can occur during any acute illness. The hallmark of the syndrome is low T3 with normal or low TSH. It is well-documented that COVID-19 can cause the release of large amounts of pro-inflammatory cytokines, thus it stands to reason that non-thyroidal illness syndrome can be caused by COVID-19 infection.
Several case reports and case series have also shown that COVID-19 can cause subacute thyroiditis. This is a primary inflammation of the thyroid that causes a mild thyrotoxic state and occurs after an upper viral respiratory infection. Inflammation and swelling of the thyroid causes stretching of the thyroid capsule, which leads to pain in the thyroid in the classic variant with mild thyroid hormone elevations. There is also an atypical variant of subacute thyroiditis that does not cause pain, but has similar thyroid dysfunction.
This less common variant of subacute thyroiditis does not cause pain in the thyroid, usually occurs following pregnancy, and is thought to be an autoimmune thyroiditis. Both typical subacute thyroiditis and atypical subacute thyroiditis have been reported in COVID-19 patients. Hyperthyrotoxicosis has also been reported in COVID-19 patients. This is expected considering that upwards of 50% of subacute thyroiditis patients show signs of overt thyrotoxicosis.
It is unclear if viral subacute thyroiditis is due to direct infection of the gland by the virus, or if it is a reaction to cytokines released during the viral infection. The SARS-CoV-2 virus enters human cells through the ACE2 receptor. Thyroid follicular cells express the ACE2 receptor, thus making thyroid tissue a possible target of direct infection by the SARS-CoV-2 virus.
Main takeaways are:
1) pre-existing thyroid dysfunction does not lead to an increased COVID-19 infection rate or a worse prognosis during a COVID-19 infection
2) COVID-19 can cause acute hypothyroidism via the non-thyroidal illness syndrome
3) COVID-19 can cause subacute hyperthyroidism, and
4) COVID-19 can cause overt thyrotoxicosis via direct inflammation of the thyroid. Long-term most acute thyroid dysfunction resolves once the patient has cleared the COVID-19 infection.
Biotime offers several thyroid hormone biomarkers, such as: TSH, TT3, fT3, TT4 and fT4. their unique clinical utilities provide great deal of making precise decisions for physician in place. Clinical utilities including:
1. As an aid in the screening, clinical diagnosis, prognosis and therapeutic effect evaluation of thyroid diseases.
2. As an aid in the diagnosis of primary hyperthyroidism and primary hypothyroidism.
3. First strategy for abnormal thyroid function diagnosis.
4. Screening newborns for hypothyroidism
5. Screening of TSH levels during pregnancy
Reference
World Health Organization
American Thyroid Association
Raymon Grogan et al
Hossain et al Front Pharmacol 16(11):563478.
Parolin et al Endocr Metab Immune Disord Drug Targets. doi.10.2174/1871530320666200905123332
Marazuela M et al Rev Endocr Metab Disord 21(4):495–507.
Rotondi M, et al J Endocrinol Invest 6:1–6. doi.10.1007/s40618-020-01436-w
Xiamen Biotime Biotechnology Co., Ltd. https://www.xiamenbiotime.com/
Previous :
Is PCT Tonic Response in COSTY SEPSIS?Next :
Thyroid, How Much Do You Know?