How
Productive is the D-Dimer for Chest Pains and Covid-19?
D-dimers are cleavage products of fibrin
that occur during plasmin-mediated fibrinolysis of blood clots. In the
emergency department, D-dimer tests are broadly used as an excellent non-invasive
triage biomarker in patients, which measurement represents a valuable and
cost-effective tool in the differential diagnosis of acute chest pain including
the main life-threatening entities: acute coronary syndrome, pulmonary
embolism, and acute aortic syndrome. Whereas the diagnostic and prognostic
values of D-dimer testing in acute coronary syndrome is of less priority,
increases of D-dimers are frequently found in venous thromboembolism and acute
aortic syndromes, especially acute aortic dissection.
Laboratory evaluation
D-dimer levels can be assessed by
microplate enzyme-linked immunosorbent assay, enzyme-linked immunofluorescence
assay, whole-blood cell agglutination, or latex agglutination tests. The
sensitivity, specificity, and negative predictive value of D-dimer tests depend
on the kind of used test, the cutoff value, and the kind of assumed disease.
Cutoff levels are influenced by the kind of test used and may differ between
different laboratories. D-dimer levels are associated with the amount of
clotted blood. Highest levels are reached in massive venous thromboembolism and
after cardiovascular arrest.
Influence of D-Dimers on ACS
Acute myocardial ischemia is caused by
thrombotic occlusion of coronary arteries, implicating that D-dimer levels
should be raised in focal coronary thrombosis. Whereas troponin is a highly
sensitive and specific parameter for myocardial injury, elevation is measurable
not until 3-4 hours after onset of symptoms. By contrast, D-dimer propose
earlier rise than common markers of cardiac injury. It has been demonstrated
that increased D-dimer levels may serve as an independent diagnostic marker for
myocardial infarction with an increase in diagnostic sensitivity of the
electrocardiogram and clinical history plus D-dimer.
Value of D-Dimer Measurement in PE
D-dimers have been shown to be highly
sensitive in venous thromboembolism. Owing to the fact that deep vein
thrombosis and pulmonary embolism often occur at the same time and up to 50% of
patients with deep vein thrombosis have clinically inapparent pulmonary
embolism, D-dimer levels can be used similarly in patients with deep vein
thrombosis and pulmonary embolism. Therefore, the D-dimer test as a fast and
cost-effective method is recommended in suspected pulmonary embolism.
D-Dimers in Aortic Dissection and other
Aortic Syndromes
The term acute aortic syndrome includes
different conditions ranging from an intramural hematoma to typical aortic
dissection, together characterized by a disruption of the structural integrity
of the aortic wall with subsequent initiation of coagulation. Apart from
clinical presentation, imaging methods, and other biomarkers, D-dimers might be
of diagnostic as well as prognostic value. It has been shown that a positive
D-dimer test has a sensitivity of about 97%, a specificity of 56%, a positive
predictive value of about 60%, and a negative predictive value of up to 96%.
Role of D-Dimer During the Pandemic
COVID-19 has caused health equipment
shortages worldwide, and the allocation of scarce resources is problematic and
presents with many ethical problems. To provide the most benefit to COVID-19
patients, there is an increasing need to better allocate these scarce
resources. Raised D-dimer level is considered a poor prognostic feature for
COVID-19 patients. More recently, according to a pooled analysis study,
increased D-dimer values were frequently found in patients with a severe
COVID-19, suggesting that this biomarker has a promising potential for
determining mortality. Few studies have also reported an increased risk of
mortality in COVID-19 patients with elevated on-admission D-dimer levels.
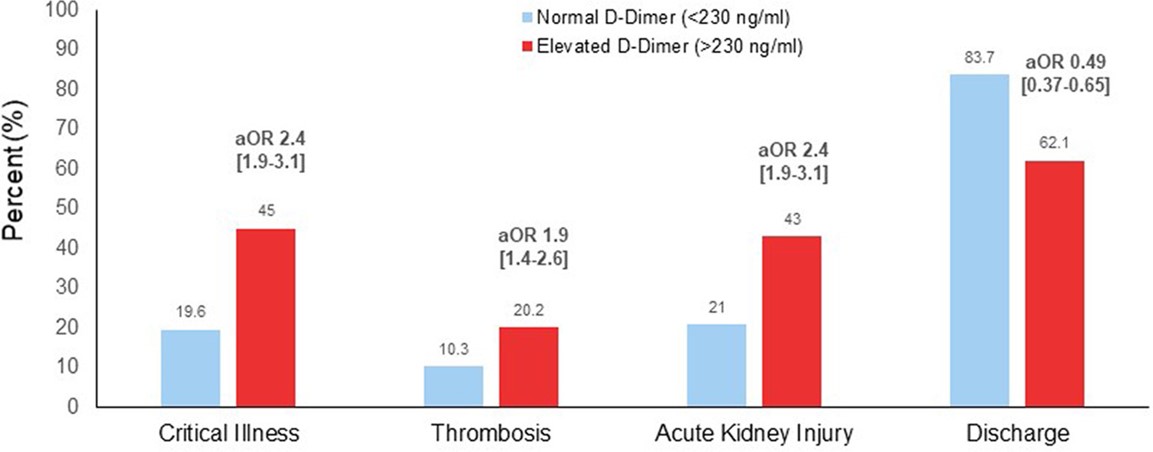
Baseline D-dimer measurements and adverse events. aOR indicates adjusted odds ratio.
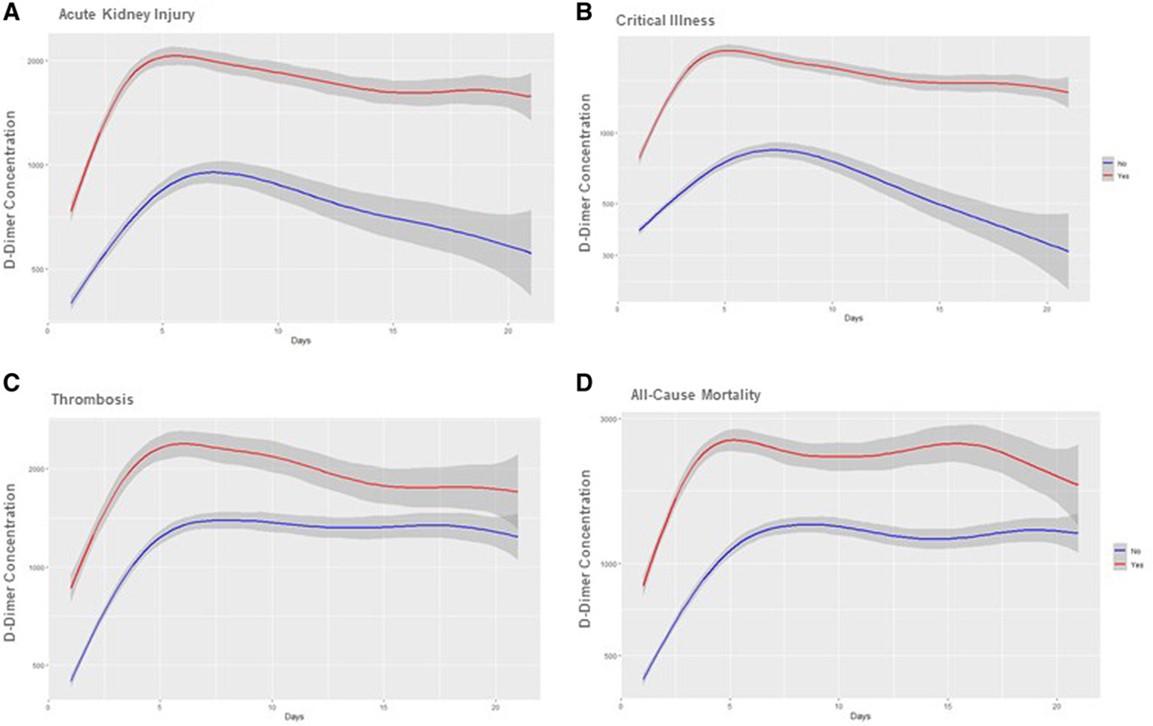
Trajectory of D-dimer during the first 21 d of
hospitalization. Patients are stratified by (A) acute kidney injury, (B) critical illness, (C)
thrombosis, and (D)
all-cause mortality.
COVID-19 at 4 hospitals within a large health
system in New York City, 1823 (76%) had evidence of elevated D-dimer above the
laboratory-specific upper limit of normal at hospital presentation and 2049
(86%) had an elevated D-dimer at any point during the hospitalization before
discharge. Outcomes of patients with elevated D-dimer at the time of admission
were particularly poor, with 45% critically ill, 20% with thrombosis, and 43%
with acute kidney injury. D-dimer level was independently associated with these
outcomes after multivariable adjustment for demographics, clinical
characteristics, and other biomarkers that we have previously shown are
associated with adverse outcomes. In contrast, individuals without an elevated D-dimer at
presentation were more likely to be discharged without developing a critical
illness.
Conclusions
D-dimer as a marker for activation of
coagulation system is a fast and cost-effective parameter used in emergency
medicine in the discrimination of acute thoracic pain. Furthermore, D-dimer
level on admission has a promising prognostic value for predicting all-cause
mortality of COVID-19 patients. Despite the differences in threshold values
across the studies, there was a roughly fivefold increase in all-cause
mortality for patients with elevated D-dimer levels on admission compared to
normal level.
References
Di
Nisio, M. , Squizzato, A. , Rutjes, A.W. , Buller, H.R. , Zwinderman, A.H. ,
Bossuyt, P.M. Diagnostic accuracy of D-dimer test for exclusion of venous
thromboembolism: A systematic review. J Thromb Haemost. 2007; 5(2): 296–304.
Google Scholar | Crossref | Medline | ISI
Sadosty,
A.T. , Goyal, D.G. , Boie, E.T. , Chiu, C.K. Emergency department D-dimer
testing. J Emerg Med. 2001; 21(4): 423–9. Google Scholar | Crossref
Koracevic,
G.P. Pragmatic classification of the causes of high D-dimer. Am J Emerg Med.
2009; 27(8): e5–1016. Google Scholar | Crossref
Steurer,
J. , Held, U. , Schmid, D. , Ruckstuhl, J. , Bachmann, L.M. Clinical value of
diagnostic instruments for ruling out acute coronary syndrome in patients with
chest pain: A systematic review. Emerg Med J. 2010; 27(12): 896–902. Google
Scholar | Crossref | Medline | ISI
Bayes-Genis,
A. , Mateo, J. , Santalo, M. . D-dimer is an early diagnostic marker of
coronary ischemia in patients with chest pain. Am Heart J. 2000; 140(3):
379–84.
Bounameaux,
H. , Slosman, D. , de Moerloose, P. , Reber, G. Diagnostic value of plasma
D-dimer in suspected pulmonary embolism. Lancet. 1988; 2(8611): 628–9. Google
Scholar | Crossref
Goldhaber,
S.Z. , Vaughan, D.E. , Tumeh, S.S. , Loscalzo, J. Utility of cross-linked
fibrin degradation products in the diagnosis of pulmonary embolism. Am Heart J.
1988; 116(2 pt 1): 505–8. Google Scholar | Crossref
Janssen,
M.C. , Wollersheim, H. , Verbruggen, B. , Novakova, I.R. Rapid D-dimer assays
to exclude deep venous thrombosis and pulmonary embolism: Current status and
new developments. Semin Thromb Hemost. 1998; 24(4): 393–400. Google Scholar |
Crossref | Medline
Parthenakis,
F. , Koutalas, E. , Patrianakos, A. , Koukouvas, M. , Nyktari, E. , Vardas, P.
Diagnosing acute aortic syndromes: The role of specific biochemical markers.
Int J Cardiol. 2010; 145(1): 3–8. Google Scholar | Crossref
Weber,
T. , Högler, S. , Auer, J. . D-dimer in acute aortic dissection. Chest. 2003;
123(5): 1375–8. Google Scholar | Crossref
Shimony,
A. , Filion, K.B. , Mottillo, S. , Dourian, T. , Eisenberg, M.J. Meta-analysis
of usefulness of D-dimer to diagnose acute aortic dissection. Am J Cardiol.
2011; 107(8): 1227–34. Google Scholar | Crossref
Rosenbaum,
L (2020) Facing Covid-19 in Italy – ethics, logistics, and therapeutics on the
epidemic's front line. The New England Journal of Medicine 382,
1873–1875.CrossRefGoogle ScholarPubMed
Truog,
RD, Mitchell, C and Daley, GQ (2020) The toughest triage – allocating
ventilators in a pandemic. The New England Journal of Medicine 382,
1973–1975.CrossRefGoogle ScholarPubMed
Tang,
N et al. (2020) Abnormal coagulation parameters are associated with poor
prognosis in patients with novel coronavirus pneumonia. Journal of Thrombosis
and Haemostasis 18, 844–847.CrossRefGoogle ScholarPubMed
Petrilli
CM, Jones S, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y, Tobin KA, Cerfolio
RJ, Francois F, Horwitz LI. Factors associated with hospital admission and
critical illness among 5279 people with coronavirus disease 2019 in New York
City: prospective cohort study.BMJ. 2020; 369:m1966.CrossrefMedlineGoogle
Scholar